The most up-to-date information for all things AAST
Expand to Explore
Editor's Note: November 2025
Editor's Note
Written by: Shannon M. Foster, MD
Friends and Colleagues: A call for awareness on the night of All Hallows. Saints or sinners, we all need protection, prevention, preparation, and compassion. Please read on:
Halloween’s Hidden Toll: Honoring Injury Prevention and Trauma Teams Around America’s Most Dangerous Night
Halloween, with its blend of folklore, festivity, and fantasy, remains one of the most culturally resonant nights of the American calendar. But for those of us in injury prevention, public health, and injury management, it is also a night of heightened vigilance—a convergence of environmental hazards, behavioral risks, and systemic strain. The data is clear: October 31st consistently ranks among the most injury-prone nights of the year.
From Samhain to Surveillance: A Legacy of Protection
Halloween’s roots stretch back to the Celtic festival of Samhain, a ritual marking the end of harvest and the beginning of winter. Ancient communities believed the veil between the living and the dead thinned on this night, prompting protective customs—bonfires, disguises, and offerings. Today, those traditions echo in our costumes and candlelit jack-o’-lanterns, but the spirit of protection lives on in a different form: coordinated public health strategies, community education, and data-driven interventions.
Injury Patterns That Persist
Halloween continues to present unique predictable injury patterns:
- Over 3,200 emergency department visits with lacerations from pumpkin carving, fall-related trauma, and burns from flammable costumes and decorations leading the list.
- Pedestrian fatalities triple, especially among children, due to poor visibility, distracted driving, and high foot traffic.
- Poisoning incidents spike by 13%, often involving unsafe candy or ingestion of non-edible items mistaken for treats.
- Alcohol-related injuries and DUIs surge among adults, contributing to motor vehicle collisions, falls, and interpersonal violence.
Children remain disproportionately vulnerable on Halloween. The spike in pedestrian injuries alone demands attention, and many of you have responded with combinations of reflective gear distribution, safe route mapping, school-based education campaigns, cross-sector collaboration with law enforcement, transportation agencies, and frontline healthcare workers.
These efforts save lives and exemplify the best of community-centered public health.
Adult Behaviors and Systemic Load
For adults, Halloween is strongly associated with high-risk behaviors—alcohol consumption, impaired driving, and crowd-related trauma. Substance use incidents requiring health care interventions drastically rise. Sexual assault presentations spike during the large-scale celebrations that allow the intersection of anonymity and intoxication. Yet through coordinated messaging, sober ride programs, buddy-system events, and venue partnerships, many communities are reversing the trend and reducing rates of preventable harm.
Your work in these spaces—whether through policy, outreach, surveillance, and surge readiness — IS transforming Halloween from a reactive crisis into a proactive model of injury prevention and injury management. Take a moment to recognize the entire public health engine at work in each one of our communities and trauma centers:
- data analysts who track injury trends and inform policy.
- educators who teach children how to stay visible and safe.
- volunteer coalitions that distribute gear, map safe routes, and engage in neighborhoods.
- emergency responders who prepare and respond with compassion and skill.
- public health leaders who see the patterns, build the partnerships, and drive action in a change-resistant environment.
Trauma Teams: The Final Line of Defense
As the surge of Halloween-related injuries unfolds, trauma surgeons and trauma teams stand as the final safeguard in the continuum of care. Your expertise transforms the Halloween chaos into coordinated response. Please ensure you are ready.
To every trauma surgeon, trauma nurse, trauma advanced practitioner, and every clinical and administrative team member stepping into the fray with skill and compassion: you carry forward the legacy of protection that Halloween once symbolized—and you do it with excellence.
Thank you.
Shannon
President's Message: November 2025
President's Message
Written by: Kimberly A. Davis, MD, MBA
Thank you to all our members and guests who attended the 84th Annual Meeting in Boston – our attendance was truly memorable! Congratulations to Dr. Nirula and the entire Program Committee for organizing an enjoyable and educational event. There were many highlights, including the incredible Fitts Oration by Dr. Brian Eastridge titled “Forged in the crucible of life and death: Build upon legacy and bound by mission.” His speech was a compelling and inspiring tribute to our military members and their sacrifices in service to our country. Other notable moments included Dr. Ronny Stewart’s Presidential Address on lessons learned from trauma system development and the panel session on the development of NTEPS. It was an exceptionally successful meeting, and I thank everyone who contributed to its creation and execution.
As we anticipate the coming year, there is much work ahead. All our committees are busy with new and ongoing projects. Thankfully, this year we welcomed more than 75 new Fellows and 87 Associate Members into the organization. Additionally, we successfully placed over 90 members in new committee positions. Three new committee chairs were appointed including Mitch Cohen (Scholarship), Bindi Naik-Mathuria (Pediatric Trauma) and Shannon Foster (Communications). If you volunteered, you were assigned to a committee. We look forward to your participation in the organization. Feedback and input from our members make us a stronger, more cohesive organization.
As I am sure you will hear from Suresh Agarwal, our REF Chair, we had a very successful auction at the banquet. We sincerely appreciate our members' generosity in supporting the REF. Strengthening and augmenting the research engine of the organization's is one of my main priorities for the upcoming year, and I have great faith in our committee chairs and their ability to facilitate this goal, including Mitch Cohen (inaugural Scholarship Chair) and Kevin Schuster (MIT). More details will come soon, as they have some exciting ideas to share.
In other news, we welcome our third class to the Leadership Academy, led by Bellal Joseph, and celebrate the ongoing success of the ROBO-TRACS course under Matt Martin's leadership. More updates on future educational offerings to come…
Finally, I am incredibly grateful to Sharon Gautschy and the outstanding AAST staff who make all our work possible. We are fortunate to have such a talented team that consistently works behind the scenes to keep our projects moving forward. Please remember to thank them during your committee conference calls... chances are they planned them! And from me, a personal thank you for the honor of serving as your President for the upcoming year.
My best,
Kim
Executive Director's Note: November 2025
Executive Director's Note
Written by: Sharon Gautschy, AAST Executive Director
Thank you to everyone who attended the 84th Annual Meeting of AAST and Clinical Congress of Acute Care Surgery. Over 1,400 attendees, including exhibitors, guests, and on-demand participants, registered for the event. We are already looking forward to next year.
The 85th Annual Meeting of AAST will be held from September 16-19, 2026, in Dallas, TX. Please save the date. As some may know, the 2026 meeting was initially scheduled at the Hilton San Francisco. Unfortunately, the Hilton San Francisco asked AAST to move our meeting because a much larger event was coming to town during our meeting dates, and that event wanted to buy out the entire hotel. While the Hilton San Francisco could have hosted AAST if we had stayed, the bigger event would have been a distraction for AAST and its attendees. In early 2025, AAST sent a Request for Proposal (RFP) to all the major hotel chains to find available properties. Only three properties met AAST’s requirements: two in Dallas and one in California. The Board ultimately selected the Dallas property because it offers easier access than Anaheim.
We look forward to seeing you there!
Calling all in-training fellows and attendings – the AAST Research Scholarship portal opens November 17! Applications are due by February 3, 2026. Please collaborate with your faculty to submit your research proposal. AAST aims to award as many scholarships as possible, but we need well-developed research projects. You can find the scholarship application in the “Professional Development” tab of the AAST website.
Start planning your abstract for the meeting now. The abstract system opens December 1st and closes February 15th. Get your abstract ready for AASTReview! As a reminder, AASTReview is a program where a select group of AAST members will volunteer as mentors to assist abstract submitters in refining their work.. AAST members can volunteer to be a mentor and/or mentee, and non-members can apply to be mentees. The program details will be sent to all members in early December. This is a service AAST offers its members, so please utilize it!
Please whitelist emails from [email protected]. AAST sends out a weekly email with important dates and information related to the association. We want you to participate.
Have a great holiday season!
Associate Membership Chair Message: November 2025
Associate Membership Chair Message
Written By: Brittany Bankhead, MD, MS, FACS
What an incredible time we had at this year’s AAST Annual Meeting! It was energizing to connect with so many Associate Members in person, and the excitement surrounding the Associate Member community was truly palpable. Our group celebrated both the most well-attended business meeting and happy hour in our history — a clear reflection of the enthusiasm, ideas, and camaraderie that make this organization so special.
As we move into fall, one of our headline initiatives is The Sounding Board, a new mentorship program designed to provide focused, high-impact guidance for members at all stages of their careers. This effort grew directly from a member-wide survey that highlighted a strong desire for senior mentorship in research and professional development. Sign-ups will be offered quarterly to allow new mentor-mentee pairings. You can learn more and sign up on the website.
Beyond the Sounding Board, there are many ways to stay connected and involved. Our WhatsApp groups remain active spaces for sharing everything from clinical questions and research opportunities to parenting tips and cooking ideas — a true reflection of how multidimensional and supportive this community is. And if you’re interested in contributing but unsure where to start, reach out to one of our committee chairs. There are always ad hoc projects and initiatives where your expertise and enthusiasm are welcome.
We’re grateful for the energy, collaboration, and innovation that Associate Members bring to the AAST, and to the Board of Managers for their continued support and guidance in helping shape the next generation of trauma surgeons.
Brittany Bankhead, MD, MS, FACS
Chair, AAST Associate Membership
Announcing the Sounding Board: A New Mentorship Initiative
Multi-Institutional Trials Committee
Announcing the Sounding Board: A New Mentorship Initiative
Written By: Navpreet K. Dhillon, Kevin Schuster, and Mayur Patel
This summer, a member-wide survey of AAST highlighted a clear theme: trainees (resident, fellow), junior faculty, and mid-career faculty are eager for senior mentorship in research and professional development.
In response, the Associate Member Council and the Multicenter Trials Committee have launched the Sounding Board: brief, high-impact mentorship sessions designed to engage on topics in research and professional development.
Through the program, interested AAST members (of any category) are matched with one or two senior AAST members for a single focused, one-hour mentorship session. Conversations may cover a broad range of topics—from developing a research niche or refining a study to topics in professional development, such as navigating career transitions and trajectories. Mentees will provide a brief report to the AAST following each session to share insights from their experience.
Sign-ups will be announced quarterly to create new mentor-mentee pairings. This is a great opportunity to interface with a senior member of the AAST and have a focused discussion around a topic of your preference.
Senior and experienced AAST members are critical to the success of this initiative – please consider serving as a Mentor!
Please visit the Sounding Board website here.
Questions may be directed to Dr. Navpreet Dhillon at [email protected].
Healthcare Economics Update
Healthcare Economics Committee
Healthcare Economics Update
Contributing Author: Parker Hu, MD, FACS
Managing Editors: Raeanna Adams, MD, MBA, FACS; Samir Fahkry, MD, FACS
Telemedicine
Unfortunately, the telemedicine waiver present during the pandemic has now expired and there was no successful legislative Continuing Resolution to extend the conditions. As of October 1, 2025, we must adapt to the former criteria for reimbursement. Mental health services will still be covered, regardless of originating site, but will return to requiring an in-person followup within 6 months. Patients receiving other covered telehealth services must once again be at an approved originating site of a rural area, as defined by the Center for Medicare Services (CMS).
Correctly Combining Codes for Procedures on Same Date
Basic Rules
CMS created the National Correct Coding Initiative (NCCI) to prevent payment of services that should not be reported together. This prevents payments for overlapping services except where “separate and distinct.”
- In general, providers must report:
- Services correctly without either upcoding or downcoding.
- The most comprehensive service.
- Complete procedural codes, not separate, individual fragments. In other words, services integral to a procedure cannot be separately billed. Common examples of elements that cannot be separately billed for many procedures include:
- Incision
- Exploration of surgical field
- Lysis of adhesions
- Intra-operative endoscopy when used to verify operation performed correctly without injury/leak
- Cultures
- Insertion of drains
- Closure
- A single approach for procedure
- Multiple approaches for same procedure are mutually exclusive.
- In other words, if an initial approach fails (i.e. laparoscopic converted to open), only the completed approach to procedure may be reported (in this example, only the open procedure can be billed)
- Conversion to open from a laparoscopic approach cannot be billed as separate diagnostic laparoscopy
- A single complexity for a procedure, unless at different anatomic locations or encounters
NCCI Modifers
CPT modifiers can facilitate reimbursement for multiple codes when appropriate. Use of these modifiers during the same encounter should only be for procedures not ordinarily performed on the same day. Use can’t be described by a more specific modifier.
- Modifier -58: Staged or Related Procedure During Postoperative Period
- If second procedure was:
- Planned prospectively
- More extensive than first procedure
- Performed after a separate diagnostic procedure
- Diagnostic endoscopic procedure leading to open operation may both be reported with -58.
- However, diagnostic endoscopy may never be combined with another endoscopic procedure in same organ/region.
- Similarly, diagnostic laparoscopy may not be combined with another laparoscopic or, if converted, open operation
- Diagnostic endoscopic procedure leading to open operation may both be reported with -58.
- If second procedure was:
- Modifier -59: Separate and Distinct Services
- Indicates a procedure was distinct or independent from other procedural services performed on the same day.
- Documentation must support that services are distinct and appropriate due to:
- A different session,
- Eg. Resuscitative thoracotomy in ER then later laparotomy in OR
- A different procedure or surgery,
- Eg. Splenectomy and concurrent right hemicolectomy
- NOT cecectomy and right hemicolectomy
- A different site or organ system,
- Eg. Multiple different areas of bowel requiring separate repair/resection
- NOT anterior and posterior injuries of one segment of bowel
- A different incision,
- Eg. Patient with both thoracotomy and laparotomy
- Or a separate injury
- A different session,
- Similar, more specific modifiers are also available and should be used if possible:
- XE: separate encounter - a service that is distinct because it occurred during a separate encounter
- XP: separate practitioner - a service that is distinct because it was performed by a different practitioner
- XS: separate structure - a service that is distinct because it was performed on a separate organ/structure
- XU: unusual non-overlapping service - the use of a service that is distinct because it does not overlap usual components of the main service
- Modifier -78: Unplanned Return to Operating Room for Related Procedure
- Complication requiring return to OR during the global period of initial operation
- Modifier -50: Bilateral Procedures
- Second procedure occurs during same session on opposite side
- Modifier -51: Multiple Procedures
- Used to indicate that multiple procedures were performed by the same provider during the same session
- If two procedures are distinct and not bundled by NCCI.
- Should not append to add-on codes (designated by “+” sign)
- Typically reimbursed 100% of allowable amount for primary procedure and reduced rate for subsequent procedures.
- No longer required by Medicare and some other payors.
References
- Medicare payment policy. Telehealth.HHS.gov. May 29, 2025. https://telehealth.hhs.gov/providers/billing-and-reimbursement/medicare-payment-policies
- Telehealth & Remote Patient Monitoring. Medicare Learning Network MLN901705. April 20, 2025. https://www.cms.gov/files/document/mln901705-telehealth-remote-patient-monitoring.pdf
- NCCI Policy Manual for Medicare Services. Chapter 1 – General Correct Coding Policies. Revision Date (Medicare): 2/28/2025. https://www.cms.gov/files/document/01-chapter1-ncci-medicare-policy-manual-2025finalcleanpdf.pdf
- Proper Use of Modifiers 59, XE, XP, XS, & XU. Medicare Learning Network. MLN1783722 February 2025. https://www.cms.gov/files/document/proper-use-modifiers-59-xe-xp-xs-xu.pdf
Entrusting Compassion: Teaching Primary Palliative Care in Trauma Education
Palliative Care Committee
Entrusting Compassion: Teaching Primary Palliative Care in Trauma Education
Written By: Mackenzie Cook, MD
Every acute care surgeon can recall the moments that linger long after the operative dictation is signed: a family meeting in the ICU at 2am, the conversation where recovery slips out of reach, the silence after delivering news that a loved one has died. These discussions define our practice as much as hemorrhage control and complex critical care, yet most of us were never formally taught how to manage them. We learned by watching, by stumbling, and by improvising in real time. That approach is not good enough for the next generation.
The educational community is beginning to catch up. The newest edition of ATLS includes an entire chapter on communicating serious news in the acute setting, signaling that communication belongs alongside airway, breathing, and circulation in the trauma surgeon’s toolkit. TQIP guidelines explicitly call for trauma teams to provide primary palliative care, recognizing that timely involvement improves quality of care. The Fundamentals of Communication in Surgery curriculum, developed by Dr. Schwarze and colleagues at the Wisconsin Patient Preferences Project, is being piloted, offering an evidence-based roadmap for building these skills. The message is clear: communication and palliative care are essential competencies of acute care surgery.
We already know how to teach complex, high-stakes skills. We scaffold, supervise, and entrust in the operating room and trauma bay. That same logic should apply to palliative care skills. Instead of waiting for a new EPA to be created, we can borrow the concept of entrustment directly; progressively giving trainees autonomy to lead goals-of-care conversations, to deliver serious news, and to manage distressing symptoms. By the end of fellowship, acute care surgeons should be fully entrusted to handle these encounters independently, just as we trust them to run an ICU or perform a trauma laparotomy.
Teaching palliative care is not easy for every surgeon. Skill varies widely, and many faculty do not have an established deliberate approach to teaching these conversations. The good news is that resources already exist. The SCORE curriculum includes modules specifically for surgical residents, and the VitalTalk group has proven that difficult conversations can be practiced through simulation. The infrastructure is in place; what remains is our desire to use it. Critically, this is not the responsibility of “the system” alone. Each of us, as individual educators, must take up the charge to incorporate palliative teaching intentionally into our daily work with partners, colleagues, students, residents and fellows.
The practical steps are straightforward. Start early and repeat often. Let interns observe and learn basic communication frameworks. By mid-residency, give them opportunities to practice in simulations or low-stakes clinical settings. By senior years, entrust them to lead conversations under direct or indirect supervision. Challenge colleagues to view high quality primary palliative care as an essential part of our job that deserves professional development and quality assurance. In short, teach this skill like you teach all the others. Perhaps the most difficult step connects to this final point - faculty must role model these skills and demonstrate, visibly and repeatedly, that providing high quality primary palliative care is an essential part of being a high quality surgeon.
We are uniquely credible teachers of these skills for trainees as we live them daily. We sit at the intersection of sudden catastrophe and life-altering decision-making. Our trainees watch how we deliver devastating news, how we balance honesty with compassion, and how we acknowledge uncertainty while guiding a path forward. We already have the curricula, the guidelines, and the educational frameworks. What we need now is resolve.
If trauma education is to remain at the forefront of surgical training, we must expand our definition of technical mastery to include communication and compassion. By embedding palliative education into the fabric of residency and fellowship, we will graduate surgeons prepared not only to save lives, but also to guide patients and families through their hardest moments with skill and humanity.
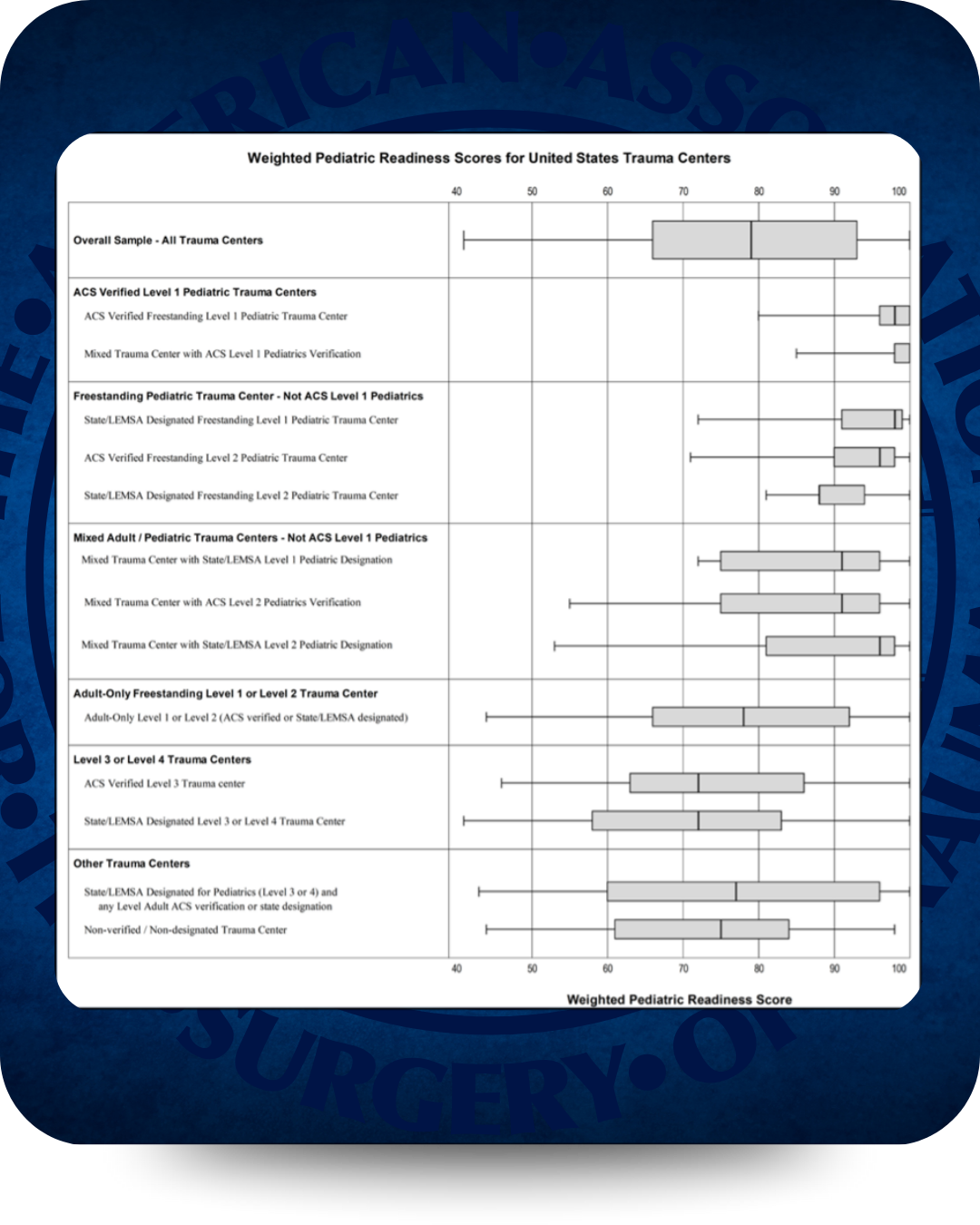
What is “Peds Ready” and how can your ED get there?
Pediatrics Committee
What is “Peds Ready” and how can your ED get there?
Written By: Aaron R. Jensen, MD, MEd
Children have unique characteristics that require specific care, especially in emergencies. But not all children have access to specialized pediatric care. In fact, 80% of children receive emergency/trauma care in general EDs. Low pediatric patient volume can make it challenging to prioritize pediatric care.
Pediatric Readiness saves lives. Research shows that high levels of Pediatric Readiness (>87 points) are associated with:
New ACS trauma center verification for Level 1 and 2 centers requires being “Peds Ready” (National Pediatric Readiness Project assessment), which has improved readiness for these centers; however, adult only free-standing level 1/2 centers, level 3 and 4 centers and non-designated centers, which do not have these requirements in place, still lag behind.
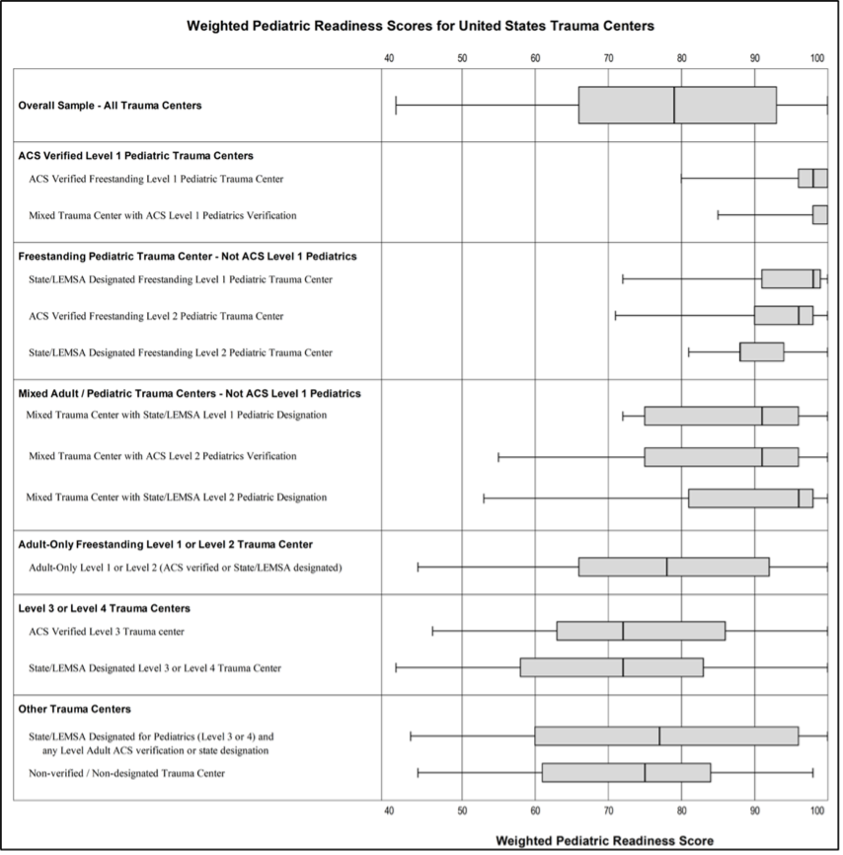
Melhado CG et al. J Trauma Acute Care Surg. 2025 Jan 1;98(1):69-77.
The EMSC’s National Pediatric Readiness Project now has simple tools to help you help your ED/Trauma Center become Peds Ready at https://emscimprovement.center/domains/pediatric-readiness-project/
Use this checklist to check your ED’s Pediatric Readiness and identify gaps.
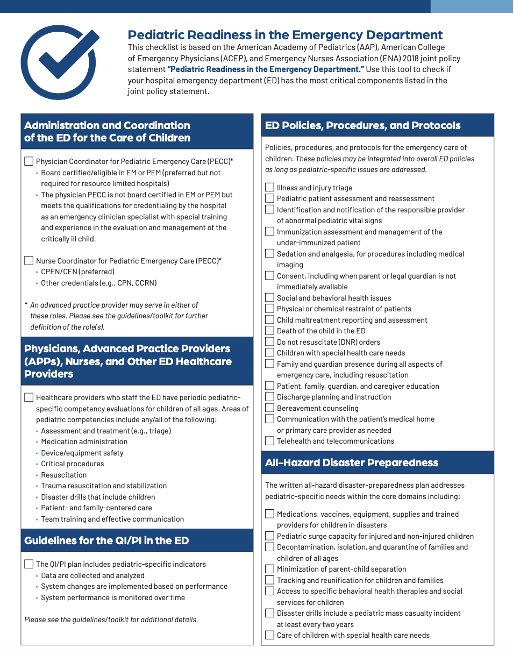

The website has FREE resources including checklists for peds equipment, supplies, medications, and protocols https://emscimprovement.center/domains/pediatric-readiness-project/readiness-toolkit/readiness-toolkit-checklist/
An additional useful resource by EMSC is their Pediatric Education and Advocacy Kit (PEAK) for Multisystem Trauma with guidelines (ex. imaging and MTP) and simulation modules found at https://emscimprovement.center/education-and-resources/peak/multisystem-trauma/?media=354

Make sure your ED/Trauma Center gets that A grade (90+) and help us save kids lives, no matter where in the country they get injured.
AAST Cutting Edge: AAST Delegation to the Kingdom of Morocco
Pediatric Committee
AAST Cutting Edge: AAST Delegation to the Kingdom of Morocco
Written By: Kristy Hawley, MD, MPH and Mary Fallat, MD
The Kingdom of Morocco hosted a delegation from the AAST to explore their country's trauma care system, medical education, and healthcare infrastructure. This meeting was initiated following a similar engagement with the American College of Surgeons (ACS) in 2022, during which the Moroccan government conveyed its interest in partnering with experts from the AAST to explore their plan to develop a comprehensive national trauma system. This delegation activity was initially scheduled in 2023; however, a large earthquake in the region prompted a delay for a year. It also afforded the delegation the opportunity to review and learn from the response to this disaster.
The delegation, led by Dr. David H. Livingston, past President of the AAST, comprised a diverse group of trauma surgeons with expertise in trauma survivorship, pre-hospital care, trauma system development, pediatric trauma, robotic surgery and post-graduate education. Activities included meetings with Morocco’s Ministry of Health and visits to prominent teaching hospitals in Rabat, Fez, and Marrakesh. The itinerary featured visits to the Mohammed VI Hospital in Marrakesh, The Mohammed V University in Rabat, and a regional hospital, Al Ghassani in Fez. Participants discussed healthcare system goals, such as improving trauma education, emergency response, and care coordination.
Morocco's healthcare system is presently undergoing significant reform, with trauma care and injury prevention as key priorities of King Mohammed VI. The Ministry of Health espouses three pillars for trauma care: prevention, trauma system development, and strengthening rehabilitation programs. The government is working to strengthen the trauma system as part of broader healthcare reforms, including the introduction of compulsory health insurance and expanded infrastructure. Moreover, Morocco's successful bid, alongside Portugal and Spain, to host the 2030 FIFA World Cup provides additional impetus to develop its trauma system to further enhance the country's emergency response services to help manage this populous event.
The next steps between the AAST delegation and the Moroccan Ministry of Health begin with preparing and delivering a formal report. This report will outline observations, findings, and insights gained during the delegation’s visit and include actionable recommendations for developing a comprehensive trauma system in Morocco. It is hoped that this will be the start of an ongoing relationship between the AAST and the Kingdom. Additionally, opportunities have been identified for potential scholarly contributions to our trauma journals from the Moroccan healthcare system, particularly through publications highlighting their unique experiences and strategies in disaster care during the 2023 Al Haouz Earthquake.
AAST Delegation Members:
Delegation Leader: David Livingston, The University of Colorado School of Medicine
Stephanie Bonne, Advocate Health Care
Mary Fallat, University of Louisville School of Medicine
Kristy Hawley, The University of Colorado School of Medicine
Katherine Kelley, Kelley Acute Care Surgery
Ajai Malhotra, The University of Vermont
Amy Murphy, TriHealth, Cincinnati
Michelle Papathanas, TriHealth, Cincinnati
Anne Rizzo, The Guthrie Clinic

Delegation members arrive at the Moroccan Ministry of Health and Social Protection in Rabat for a high-level meeting to discuss international collaboration in health policy, surgical education and trauma system development in Morocco.

Delegation members gather in the main boardroom at the Ministry of Health. Discussions focused on trauma care advancement and trauma system development.
Journal of Trauma and Acute Care Surgery Update: November 2025
Journal of Trauma and Acute Care Surgery
Journal of Trauma and Acute Care Surgery Update: November 2025
Written by: Raul Coimbra, MD, PhD, Editor-in-Chief
As you heard during the AAST Annual Meeting and in previous communications, the JTACS Impact Factor increased to 3.7 from 3.0. The Editorial Staff is very excited about this rise in the impact factor, as we have been working hard to improve the quality of manuscripts that are important to AAST, EAST, PTS, WTA, CWIS, and ANZAST members and subscribers. The two new series, "What You Need to Know" and "JTACS EGS Algorithms," have seen increased readership and website downloads. These series are ongoing. The Biostatistical Review series continues, and we thank Tabitha Garwe, Bishoy Zakhary, and Jeff Choi for organizing it.
The Journal of Trauma and Acute Care Surgery needs your help!
With the update to Windows 11 and increased firewalls at universities and medical centers, the JTACS editorial staff and board have noticed more rejections and non-deliverable emails sent to authors, editorial board members, and ad hoc reviewers. The Editorial Board has sent review invitations, and when we follow up, many of you tell us you never received them. The same thing happens with authors when we send revision letters, acceptance emails, and copyright transfer forms. To help us deliver emails more reliably to our authors, reviewers, editorial board members, and staff, we ask everyone with an account in the JTACS editorial manager to add a Gmail or another non-institutional email address for notifications. If you believe you already have an alternate email in the system, please check that it is one you monitor regularly.
Thank you,
Raul Coimbra, MD, PhD
JTACS Editor-in-Chief
Missed an Issue?
If you missed the last issue or want to revisit past content, you can browse all previous editions on our archive page. Whether you're looking for policy updates, committee highlights, or educational content, it's all there.
The Cutting Edge Podcast
Prefer to listen on the go? The Cutting Edge Podcast brings AAST to life with engaging conversations, exclusive interviews, and behind-the-scenes stories from the world of trauma and acute care surgery.
Front Line Surgery: Mastering Military Trauma Care
We’re proud to launch Front Line Surgery, a new podcast series focused on advancing readiness and expertise in military trauma surgery. Each episode features in-depth conversations with experienced military surgeons, critical case reviews, and practical strategies tailored to the challenges of battlefield care. Now streaming wherever you get your podcasts!