
Coder's Corner
by R. Lawrence Reed III, MD, FACS, FCCM & Thomas Esposito, MD, MPH
When performing a FAST examination in the trauma bay on a hemodynamically unstable blunt-trauma patient, can the procedure be billed for, and what documentation is required in the medical record?
Esposito:
 Regarding FAST exams of the abdomen, we would generally bill 76700 (WRVU's .81).
Regarding FAST exams of the abdomen, we would generally bill 76700 (WRVU's .81).
Ultrasound of the entire abdomen in real time with image documentation includes the following:
Common bile duct
Gall bladder
IVC
Kidneys
Pancreas
Liver
Spleen
Abdominal aorta
This code requires permanent documentation of ultrasound images. Images can be loaded in an electronic image storage system (e.g., PACS) or scanned into the EMR.
Written documentation detailing the exam with areas imaged (sub-xiphoid, Morrison's pouch, etc.), as well as the findings, is also required.
Reed:
 Dr. Esposito provides a response that I suspect is commonly thought of as the correct approach for billing the FAST exam. However, there are other options that bear consideration.
Dr. Esposito provides a response that I suspect is commonly thought of as the correct approach for billing the FAST exam. However, there are other options that bear consideration.
The primary problem, of course, is that there is no CPT code that is specific for the FAST exam. Accordingly, we must make do with the codes that exist and work to justify any challenges that may come to us.
The complete abdominal ultrasound code, 76000, could be seen as overcharging given that it is payment for imaging all of the structures on Dr. Esposito's list. While the FAST includes imaging of the liver, the kidney, the spleen, and the bladder, it does not routinely include imaging of the common bile duct, IVC, pancreas, or abdominal aorta, and it may or may not catch an image of the gallbladder.
The complete abdominal ultrasound exam is commonly performed in radiology or imaging suites. In this exam, the technician ensures that these structures are identified, if at all possible. Hence, in the event of an audit, given the difference in imaged structures between a FAST and the true imaging, the 76000 code could be seen as being applied inappropriately.
The components that make up a FAST exam actually include areas that would not be included in a complete abdominal ultrasound. For example, the bladder is routinely imaged in a FAST, but it is not considered part of the abdominal ultrasound; instead, it is considered to be part of the retroperitoneum. Ultrasonic imaging of the bladder is covered by CPT codes 76770 (complete retroperitoneal imaging including kidneys, aorta, nodes, ureters, and bladder) and 76775 (limited retroperitoneal exam). Also, the heart and pericardium are routinely imaged in the FAST exam, but these structures would not be covered by code 76700. The CPT code for imaging the heart and mediastinum is 76604 (ultrasound, chest [includes mediastinum], real time with image documentation). There is no specific requirement in the description for 76604 that the complete chest needs to be imaged, and there is no code for a limited chest ultrasound. And, finally, given that the entire abdomen is not routinely imaged during a FAST exam, the abdominal ultrasound code 76705 (ultrasound, abdominal, real time with image documentation; limited [e.g., single organ, quadrant, follow-up]) should be used.
Thus, billing for a FAST exam should actually use three different CPT codes: 76604, 76705, and 76775. In addition, for all ultrasound billing, the 26 modifier ("Professional Component") should be applied.
Procedural charges like ultrasound have both a professional component and a technical component. The professional component pays for the work performed by the physician in the relevant patient evaluation, performance of the study, and interpretation of the images. The technical component is payment to the institution for the purchase and maintenance of the equipment, including the process of recording and storing the images, and, when appropriate, the technician's expertise and time. The combination of the RVUs for the professional component and the technical component add up to the total RVUs for the procedure. The good news is that the work RVUs for the procedure are equivalent to the professional component; the use of the 26 modifier does not represent a further payment reduction to the physician.
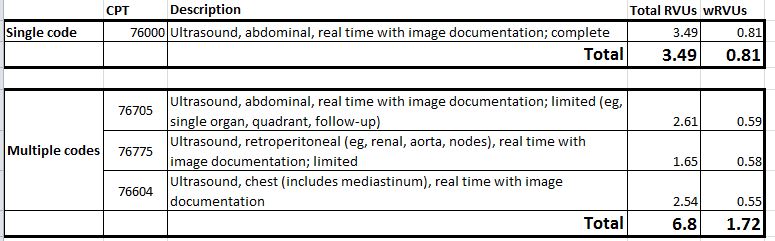
In addition to being more accurate with regard to the services actually rendered, billing three codes instead of one more than doubles the payment to the physician, as detailed in the attached chart.
Esposito:
 Without a doubt, the FAST exam sits in uncharted coding waters, and, as Dr. Reed points out, it crosses over several other ultrasound exams. However, we have not personally experienced denials using the 76700 code. We agree with the use of the 26 modifier; it is automatically attached in our system.
Without a doubt, the FAST exam sits in uncharted coding waters, and, as Dr. Reed points out, it crosses over several other ultrasound exams. However, we have not personally experienced denials using the 76700 code. We agree with the use of the 26 modifier; it is automatically attached in our system.
Depending on the payer, not all claims are reviewed. Therefore using the three-code strategy may pass through unquestioned, but there is concern that if reviewed, some or all will be denied even though the codes are not bundled. Denials for these types of radiological charges would probably go to a radiology coder for review making complete and specific documentation of exactly what was imaged even more important.
In the end, we feel code 76700 alone suffices and is a fair estimate of service. And again, it has not been denied in our experience. In our opinion, the extra effort of using three codes is a long run for a short slide that may be denied anyway.