
Coder's Corner
by R. Lawrence Reed III, MD, FACS, FCCM & Thomas Esposito, MD, MPH
Here are a scenario and questions for the next Coders’ Corner from Dr. Matthew Benns of the University of Louisville:
Called to assist urology intra-operatively on a 57 year old with a history of bladder cancer and an ileal conduit who presented with a SBO. The patient was found to have small segment of bowel necrosis intra-operatively due a peri-stomal hernia, and the surgeon performed a bowel resection and primary anastomosis; additionally, the surgeon assisted urology with re-siting of the conduit. The patient was septic and edematous and unable to be primarily closed, so he was packed and left open. Overnight in the ICU, he required critical care management in the form of ventilator adjustments and resuscitation of septic shock that was performed by the on-call intensivist (different from the operating surgeon). Further critical care management was provided the following day by the operative surgeon. The patient returned to the operative room postoperative day #2 for re-exploration and was able to be primarily closed at that time. The operative surgeon continued to provide critical care services in the form of ventilator management and weaning for an additional 2 days before the patient was extubated on postoperative day #4.
- What codes are applicable for the surgeon during the original operation?
- How should the surgeons divide and bill critical care in this case?
- How should the surgeon code the second operation?

Response from Dr. Reed:
- “What codes are applicable for the surgeon during the original operation?” The procedures identified from the narrative include:
- Bowel resection and primary anastomosis of the intestine that had become necrotic from the incarcerated hernia.
- If the intestine involved was the small bowel, CPT code 44120 (Enterectomy, resection of small intestine; single resection and anastomosis) should be used.
- Alternatively, if it was large bowel, CPT code 44140 (Colectomy, partial; with anastomosis) should be used.
- Repair of the incarcerated (actually strangulated) hernia, which was accomplished by removing the prior ileostomy (as well as the necrotic bowel) and closing the defect in the abdominal wall. The CPT code for the incarcerated hernia repair is 49561 (Repair initial incisional or ventral hernia; incarcerated or strangulated). Because it was one of other procedures, it requires modifier 51 (Multiple Procedures).
- Creation of an ileostomy at a new site.
- While there are codes for ileostomy revision, such as 44312 (Revision of ileostomy; simple [release of superficial scar]) or 44314 (Revision of ileostomy; complicated [reconstruction in-depth]), this was not what was done. Rather, the ileostomy was moved to a new site, which is most appropriately coded as CPT code 44310 (Ileostomy or jejunostomy, non-tube).
- The narrative states that the acute care surgeon is assisting the urologist with re-siting the ileostomy. There are several options available to ensure payment for both surgeons, and they all involve the use of modifiers.
- One option is to use modifier 62 (Two Surgeons). However, this modifier identifies procedures where two surgeons each perform specific aspects of the case. (A previous Coder’s Corner article discussed this issue in the placement of a ventriculoperitoneal shunt by a neurosurgeon and a general surgeon.) If the 62 modifier is used, then each surgeon receives a 60 percent payment of the total amount based upon the RVUs for the procedure; thus, there is a net 120 percent payment to the practice. However, if the 62 modifier is used, each surgeon must provide a formal operative report of their part of the procedure, and each surgeon must perform a different part of the procedure. Given that the narrative indicates that the acute care surgeon assisted the urologist in performing the re-siting, it appears that the 62 modifier solution is not appropriate because they were both working on the same aspects of the procedure simultaneously.
- Another option is to use modifier 80 (Assistant Surgeon) for the acute care surgeon. This appears more appropriate for the case described. With use of the modifier 80 by the surgeon, the urologist receives 100 percent of the payment for 44130 and the acute care surgeon receives 20 percent of the payment. Hence, the same total of 120 percent of the payment is received by the practice group.
- However, if the practice normally involves residents in surgical cases, then modifier 82 (Assistant Surgeon [when qualified resident surgeon not available]) should be used. Documentation should indicate that a qualified resident was not available in order to justify the claim. Payment for the procedure is identical to that for modifier 80 with 100 percent going to the urologist and 20 percent going to the acute care surgeon.
- “How should the surgeons divide and bill critical care in this case?” The “operative surgeon” performed critical care starting on the second day. It is not clear if we are referring to the acute care surgeon or the urologist, but it is more likely the former. Both could provide critical care on the patient as long as they are not providing it at the same time. They both are likely assigned different specialty codes, which indicates that they are not the same physician. The acute care surgeon could be assigned specialty code “02” (for General Surgery) or “81” (for Critical Care). The urologist is assigned specialty code “34” (Urology). Such co-management, if appropriately split during the day, is well documented in CMS’s Medicare Claims Manuals.
- There are two requirements to bill critical care code 99291, with or with additional 99292 codes:
- The patient must be critically ill, defined as having one or more conditions that acutely impair one or more vital organ systems such that there is high probability of imminent or life-threatening deterioration in the patient’s condition.
- In this case, the patient has acute respiratory failure (ICD-10-CM code J95.821: “Acute postprocedural respiratory failure”), which meets the definition of critical illness. However, I have found it very useful to include language in the critical care note that emphasizes this point, such as “The patient remains in critical condition requiring constant attention. He is in acute respiratory failure, which if left untreated would likely cause multiple organ failure and death. I have been monitoring his oxygenation, his arterial blood gases, and his pulmonary volumes and pressures. I have made adjustments as necessary to optimize his pulmonary function in order to ultimately wean him from the ventilator.” Language such as this is occasionally necessary to inform to coders of the severity of the patient’s clinical condition. In many electronic medical record (EMR) systems, it is possible to turn generic phrases such as the above into macros, allowing a few keystrokes to generate the entire paragraph. Obviously, specific activities and/or assessments should be included as appropriate.
- The amount of time spent on critical care for the patient (exclusive of the time spent performing procedures on the patient) must be recorded in the clinician’s critical care note. Further, in order to qualify for billing the first hour of critical care using CPT code 99291, at least 30 minutes of critical care time must be documented. Each additional half hour of critical care payment using one or more 99292s requires at least 15 minutes of additional critical care to justify the additional payment. (Again, a macro in the EMR system can be created stating “I spent _ minutes in providing critical care to this patient, excluding procedural time.” The “_” is a wild-card character in Cerner, in which hitting the F3 key on the keyboard can take you to the underscore where you can type in the specific number of minutes. Similar functions are available in other EMR systems, such as EPIC.)
- There is also a coding requirement for the fact that the operating surgeon is providing critical care on a patient that he both operated and re-operated upon. All procedures are considered to have evaluation and management (E&M) services inherent in their provision. Thus, the default attitude is that E&M services billed by a physician on a day that is within the global surgical package period for the procedure have already been reimbursed and are therefore are not separately billable. However, E&M services provided for conditions unrelated to the operation (such as pre-existing conditions) are separately billable. The use of a modifier on the E&M service’s CPT code identifies that the E&M service is unrelated to the operation. In this case, the management of the respiratory failure that justifies the provision of critical care is not due to the patient’s operation but rather to the patient’s underlying condition upon arrival. To bill CPT code 99291 and any additional 99292 codes, modifiers will need to be applied.
- In this particular case, for the first postoperative day, the surgeon should append the “24” modifier (Unrelated Evaluation and Management Service by the Same Physician or Other Qualified Health Care Professional During a Postoperative Period) as this is the first day post-op from the initial operation and therefore falls within the procedure’s 90-day global package.
- However, on the day of the take-back surgery, two modifiers are required. First, a “24” modifier should be applied because the initial global package is still in place (and will remain in place for a total of 90 days). In addition, a “57” modifier (Decision for Surgery) should be applied to the same 99291/99292 codes because the decision to reoperate on the patient occurred on the second postoperative day.
- All subsequent days on which the surgeon provides critical care will require the “24” modifier only.
- On the day the patient is extubated, critical care could be provided if the time spent in his management is 30 or more minutes. If less time is spent, however, then he no longer meets the definition of critical care, so 99291/99292 codes cannot be applied. Instead, routine daily inpatient visit codes (99231, 99232, or 99233) could be used, as long as there are other conditions present that are not included in the surgical global package and are documented in the note, such as electrolyte disorders, atelectasis, acute blood loss anemia, etc. In addition, the progress note’s payment is based upon its extent of documentation of the primary components of the note, i.e., the history, physical examination, and medical decision-making. In addition, because the E&M code is applied during the global surgical period (which now stretches 90 days beyond the second operation and not the first), a “24” modifier must be applied or the surgeon won’t be paid for his beautiful note. If there are no conditions being managed that are outside the global surgical package, then the daily visit is assumed to be paid by the surgical global package payment and therefore cannot be billed separately.
- “How should the surgeon code the second operation?”
The second operation is a relaparotomy (CPT 49002) performed during the global period of the initial operation. The CPT code should be billed with modifier 58 (Staged or Related Procedure or Service by the Same Physician or Other Qualified Health Care Professional During the Postoperative Period).
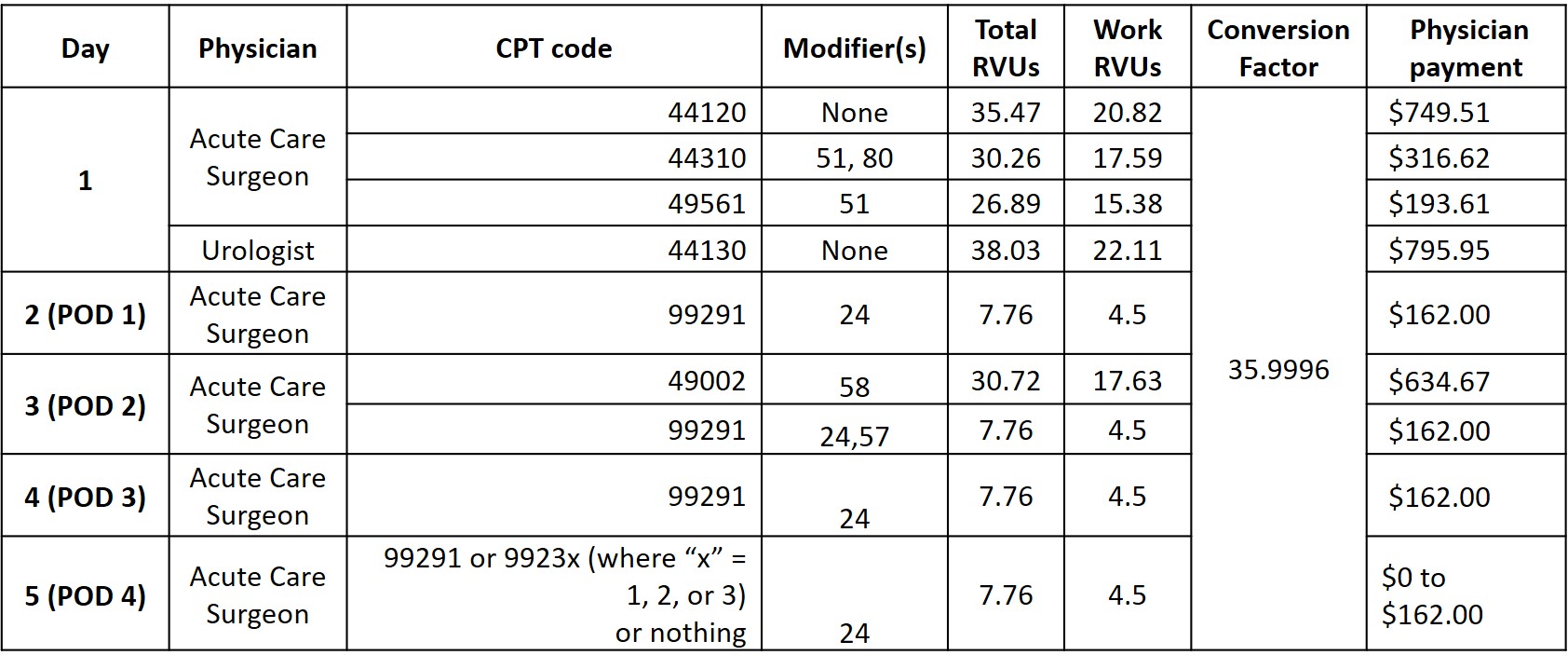
The coding and billing numbers are summarized in the Table.

Response from Dr. Esposito:
This is a complex case which Dr. Reed has thoroughly dissected in his usual fashion. Just a few points we feel are pertinent.
On the first operation, we believe the general surgeon should bill for bowel resection 44120 or 44140, depending on what was resected, as Dr. Reed points out. Both should bill for re-siting of the conduit. The urologist should bill 44314 and the general surgeon should bill the same code with the 80 modifier, and if at a teaching hospital, then the surgeon should code with an 82 modifier. If billing with the 82 modifier, the urologist must state that no qualified resident was available. Of course billing with modifiers should be based on the documentation of the “surgical choreography” or “who did what.” We assume the wound was left open, and a wound VAC applied. If that is true, then one should bill the additional code of 97605 for a wound up to 50 sq cm or 97606 if greater than 50 sq cm.
We believe that 44314 (separate procedure) is the correct, and an accurate, code for the ileostomy revision/relocation if the ileostomy is moved to new site, and therefore would not use 44310 as it might be denied. There is a small difference in RVUs garnered with 44310 being 17.59 and 44314 being 16.74.
In regards to the billing for the incarcerated hernia, per the National Correct Coding Initiative, if a hernia repair is performed at the site of an incision for an open or laparoscopic abdominal procedure, the hernia repair is not separately reportable. The hernia repair is separately reportable if it is performed at a site other than the incision, as it probably was in this case. Therefore we agree with billing 49561 using modifier 51.
Please note codes 44130 & 44314 are designated as separate procedures. This means that these are commonly carried out as an integral component of a total service. The codes designated as separate procedures should not be reported in addition to the code for the total procedure or service of which it is considered an integral component.
However, when a procedure or service that is designated as a separate procedure is carried out independently or considered to be unrelated to or distinct from other procedures/services provided at the time, it may be reported by itself or in addition to other procedures by appending modifier 59 to the specific separate procedure code to indicate that the procedure is not/was not considered to be a component of another procedure.
Of note is that our billing software indicates that 44120 and 44130 are bundled, and no modifier is allowed to unbundle. Code 44130 is an enteroenterostomy, anastomosis of intestine, with or without cutaneous enterostomy. This code includes resection with anastomosis or with ostomy and that is why it bundles with 44120 (resection with anastomosis). Similarly, 44130 is also bundled with 44310.
For the second operation, we agree with billing 49002-58.
Regarding critical charges, we agree with Dr. Reed’s detailed coding recommendations but feel the dx code Z99.11 for dependence on respirator should be added.