Description
Project: Multisociety research collaboration: timing of cholecystectomy following cholecystostomy drainage for acute cholecystitis
Authors: Konstantinos Spaniolas, MD, Daniel Dante Yeh, MD, Amanda K Arrington, MD, Todd W Costantini, MD
Background:
Biliary disease is a common surgical disease, and laparoscopic cholecystectomy is the most common and preferred strategy for the management of acute cholecystitis. Despite this, for patients who present with unfavorable systemic or local conditions, percutaneous cholecystostomy drainage is an acceptable temporizing measure. However, the rates of conversion to open cholecystectomy and associated biliary tract injury have remained significant following cholecystostomy tube drainage. In the latest Tokyo guidelines, the optimal timing of cholecystectomy following cholecystostomy drainage has been identified as an important future research question.(1) Specifically, small cohort studies (less than 100 patients each) provide insufficient information about the benefit of delayed versus early intervention following drainage.
Objective:
The aim of the study is to identify the effect of timing of cholecystectomy following percutaneous cholecystostomy drainage for cholecystitis on perioperative complication rates at interval cholecystectomy.
Research Plan:
This will be a retrospective cohort study from multiple clinical sites. Adults (age >18 years) who meet the criteria for acute cholecystitis, and who have undergone placement of percutaneous cholecystostomy tube followed by interval cholecystectomy will be included in the study cohort.
Inclusion criteria:
- Age = or > 18 years
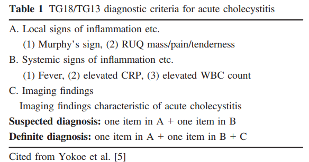
- Diagnosis of acute cholecystitis (TG18/TG13)(2)
- A. Local signs of inflammation
- Murphy Sign, RUQ tenderness/mass/pain
- B. Systemic signs of inflammation
- Fever, Elevated CRP, Elevated WBC
- C. Imaging findings suggestive of cholecystitis
- Suspected A+B
- Definite A+B+C
Exclusion criteria:
- On chronic immunosuppressive medications
- Previous history of hepatobiliary surgery
- Failure of source control following cholecystostomy drainage (i.e. cholecystectomy at the same hospitalization)
- Liver cirrhosis
- Active malignancy
- Concurrent common bile duct stones
- Transferred from another institution after cholecystostomy drainage.
Variables to be collected:
- Demographics at time of cholecystectomy
- (age, gender, weight, BMI)
- Comorbidities at time of cholecystectomy
- (charlson comorbidity index, HgA1c, previous abdominal surgery)
- Indication for drainage(1)
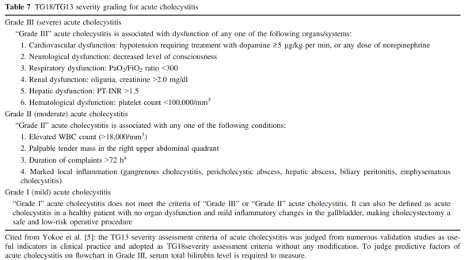
- Mild AC with severe comorbidities (CCI>6 or ASA>3)
- Moderate AC with severe comorbidities (CCI>6 or ASA>3)
- Severe AC with significant comorbidities (CCI>4 or ASA>3)
- Severe AC with negative prognostic factors (jaundice, neurologic dysfunction, or respiratory dysfunction)
- Other
- Timing from admission to drainage procedure.
- Severity of cholecystitis
- (elements of TG18/TG13 and AAST scoring system)
- Index Hospitalization data
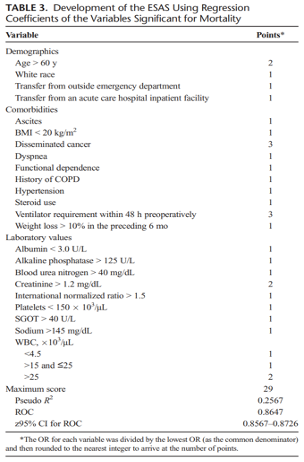
- (Total H-LOS, Total ICU-LOS, Admission-to-Drainage days, Diagnosis-to-Drainage days, Antibiotics category, Antibiotics duration, Discharge destination, Emergency Surgery Score at time of index admission)(3)
- Biliary tree imaging before cholecystectomy
- Cholangiography
- Repeat CT
- MRI/MRCP
- Patent cystic duct (yes / no)
- Atypical biliary anatomy (yes / no)
- Tube removal timing
- At cholecystectomy
- Before
- LFTs prior to cholecystectomy (values, days from labs to surgery)
- Cholecystectomy data
- (Type - lap, open, robotic, conversion, Intraoperative events, Total vs subtotal, ASA, Drain, Procedure duration, EBL, Total H-LOS, Total ICU-LOS, Discharge destination, Biliary injury, Biliary leak, Re-operation, Re-admission, ED visit, IR procedure, GI procedure)
References:
- Okamoto K, Suzuki K, Takada T, et al. Tokyo Guidelines 2018: flowchart for the management of acute cholecystitis. J Hepatobiliary Pancreat Sci. 2018 Jan;25(1):55-72.
- Yokoe M, Hata J, Takada T, et al. Tokyo Guidelines 2018: diagnostic criteria and severity grading of acute cholecystitis (with videos). J Hepatobiliary Pancreat Sci. 2018 Jan;25(1):41-54.
- Kongkaewpaisan N, Lee JM, Eid AI, et al. Can the emergency surgery score (ESS) be used as a triage tool predicting the postoperative need for an ICU admission? Am J Surg. 2019 Jan;217(1):24-28. doi: 10.1016/j.amjsurg.2018.08.002.
Appendix:
- Tokyo guidelines for diagnosis of acute cholecystitis
- Tokyo guidelines for severity grading for acute cholecystitis
- Emergency Surgery Score